Could not retrieve the oEmbed resource.
What We Learned about Federal Telehealth Programs during the First Year of the Pandemic
Recognizing how critical telehealth has been to the federal COVID-19 response, the PRAC Health Care Subgroup—which includes six federal Offices of Inspectors General—worked together to provide insights on the use of telehealth and its associated program integrity risks. Read the full report here.
Here are four things we learned:
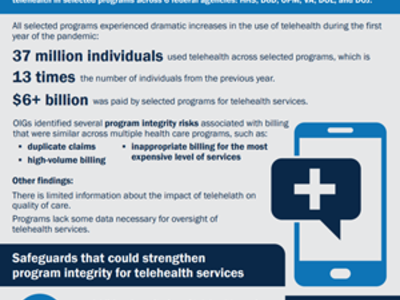
1. Telehealth use surged across federal health care programs.
During the first year of the pandemic, 37 million individuals used telehealth services across the six programs we looked at for this report. This was 13 times more than in the prior year. Federal programs paid more than $6 billion for telehealth services.
The majority of telehealth services included visits with primary care providers, specialists, and behavioral health professionals.
2. Telehealth is not without risk.
Offices of Inspectors General (OIGs) that participated in the study identified common risks of fraud, waste, and abuse associated with telehealth billing in the programs they oversee. These risks include:
- Billing for the same telehealth service twice
- Billing for extremely high amounts of telehealth services
- Inappropriately billing for the most expensive level of services
- Billing for services that were seemingly not appropriate for telehealth
3. Agencies need more data and information.
As with most of the pandemic relief programs we oversee, complete and reliable data is crucial for conducting adequate oversight. It’s also key for assessing the impact of telehealth on quality of care.
We found that there is limited information on how telehealth impacts quality of care. In addition, most of the OIGs found that, among the programs they reviewed, there is a lack of data necessary to oversee telehealth billing.
4. Agencies could use additional safeguards.
While all of the selected programs have some safeguards in place to oversee telehealth services, this report reveals that additional ones could strengthen program integrity. Here are some examples of what agencies can do to strengthen program integrity and ensure accurate payments:
- Increase monitoring of telehealth services
- Implement billing controls to prevent inappropriate payments for telehealth services
- Collect additional data
See what Inspectors General have to say:
Read the full report. See more from the Health Care Subgroup in this examination of COVID-19 testing efforts during the first seven months of the public health emergency.
What's our biggest takeaway?
Telehealth is here to stay. This report includes insights on how to safeguard the benefits of telehealth, while minimizing the risks of fraud, waste, and abuse. We hope policymakers take these insights into account when making decisions about telehealth in government programs.